In people with advanced kidney cancer, where the cancer has spread to distant organs, the cancer is usually not completely curable. The goal of treatment is therefore to make life as long and as normal as possible. Combinations of different treatments may be recommended by different doctors, including urologists, medical oncologists who prescribe anti-cancer medications, and radiation oncologists who treat people with radiation. Throughout, this team of specialists will work with you and your family doctor to help you control your symptoms and live as normal a life as possible.
Treatments for advanced kidney cancer include:
Active Surveillance (Observation):
 In some people in whom the kidney cancer has spread, the cancer might be growing so slowly that the right first option is to watch carefully. This is especially the case when the cancer has been discovered by accident. If the cancer starts to grow quickly or cause symptoms then active treatments will be recommended. A small percentage of patients might live without symptoms from the cancer for a very long time, sometimes years, so your doctor might advise you to observe for a period of time.
In some people in whom the kidney cancer has spread, the cancer might be growing so slowly that the right first option is to watch carefully. This is especially the case when the cancer has been discovered by accident. If the cancer starts to grow quickly or cause symptoms then active treatments will be recommended. A small percentage of patients might live without symptoms from the cancer for a very long time, sometimes years, so your doctor might advise you to observe for a period of time.
Surgery to remove cancer that has spread:
 In a very small number of people, the cancer spreads to only one or two places; if this is the case it can be possible to try to cut out all the metastatic cancers (a “metastectomy”). Some patients can live a very long time in these circumstances, but it really only applies to patients where there is only one or two spots elsewhere and they can all be safely removed.
In a very small number of people, the cancer spreads to only one or two places; if this is the case it can be possible to try to cut out all the metastatic cancers (a “metastectomy”). Some patients can live a very long time in these circumstances, but it really only applies to patients where there is only one or two spots elsewhere and they can all be safely removed.
Surgery to remove cancer in the kidney:
 If your health is otherwise good, there is evidence that removing the original cancer in the kidney improves survival and helps other treatments work better. This “cytoreductive” nephrectomy would be performed by your urologist (or uro-oncologist).
If your health is otherwise good, there is evidence that removing the original cancer in the kidney improves survival and helps other treatments work better. This “cytoreductive” nephrectomy would be performed by your urologist (or uro-oncologist).
Clinical Trials:
 A clinical trial is sometimes erroneously perceived as a “last resort”, but with rapidly improving treatments it should be considered the “first port of call”. A clinical trial is a way of testing new treatments, or older treatments used in a new way. Clinical trials are not right for every person; not every person is right for a clinical trial. If a clinical trial is available it can be an interesting opportunity to consider.
A clinical trial is sometimes erroneously perceived as a “last resort”, but with rapidly improving treatments it should be considered the “first port of call”. A clinical trial is a way of testing new treatments, or older treatments used in a new way. Clinical trials are not right for every person; not every person is right for a clinical trial. If a clinical trial is available it can be an interesting opportunity to consider.
Radiation therapy:
 A Radiation Oncologist uses high-energy radiation to kill cancer cells. Radiation can be very helpful if the cancer causes a lot of problems in one location, e.g. cancer in the bone causing pain, cancer in the kidney causing bleeding, cancer in the brain causing swelling. Radiation is used as a means of controlling symptoms (e.g. pain). SBRT (stereotactic body radiation therapy) is increasingly used to control kidney cancer growth.
A Radiation Oncologist uses high-energy radiation to kill cancer cells. Radiation can be very helpful if the cancer causes a lot of problems in one location, e.g. cancer in the bone causing pain, cancer in the kidney causing bleeding, cancer in the brain causing swelling. Radiation is used as a means of controlling symptoms (e.g. pain). SBRT (stereotactic body radiation therapy) is increasingly used to control kidney cancer growth.
Palliative care:
 Palliation doesn’t mean the “end of the road” or that the cancer is in its terminal stages. Palliative care is all the treatments that your team recommends to improve your symptoms and improve your quality of life. Your family doctor, your medical oncologist and your other doctors will help you with this. Sometimes palliative care physicians and nurses are consulted, and they can often provide specialised advice. Palliative treatment can improve quality of life by alleviating symptoms associated with advanced cancer.
Palliation doesn’t mean the “end of the road” or that the cancer is in its terminal stages. Palliative care is all the treatments that your team recommends to improve your symptoms and improve your quality of life. Your family doctor, your medical oncologist and your other doctors will help you with this. Sometimes palliative care physicians and nurses are consulted, and they can often provide specialised advice. Palliative treatment can improve quality of life by alleviating symptoms associated with advanced cancer.
Alternative Therapies:
 Everyone wants the best health care for themselves and their loved ones. If there are no suitable standard medical therapies available, “alternative” therapies might be proposed by well-intentioned friends, relatives or internet web-pages. These are called “alternative” because they have not been scientifically proven to shrink cancers or help patients. Worse still, they might have been proven not to help or to even cause harm. Examples of unhelpful or harmful alternative “treatments” include mega-dose vitamins, herbal products or extreme diets. Some alternative therapies can interfere with medicines normally prescribed by a doctor, causing harm to the patient. So it’s important to inform your doctor or nurse if you are considering these therapies.
Everyone wants the best health care for themselves and their loved ones. If there are no suitable standard medical therapies available, “alternative” therapies might be proposed by well-intentioned friends, relatives or internet web-pages. These are called “alternative” because they have not been scientifically proven to shrink cancers or help patients. Worse still, they might have been proven not to help or to even cause harm. Examples of unhelpful or harmful alternative “treatments” include mega-dose vitamins, herbal products or extreme diets. Some alternative therapies can interfere with medicines normally prescribed by a doctor, causing harm to the patient. So it’s important to inform your doctor or nurse if you are considering these therapies.
Complementary Therapies:
On the other hand, complementary therapies can “complement” established medical treatments, improving quality of life and symptoms. These include mindfulness meditation, relaxation techniques, remedial massage therapy, psychotherapy, prayer, yoga, acupressure and acupuncture. If there were any chance that the kidney cancer has spread to bones, chiropractic or osteopathy would not be a good idea.
Targeted Therapy
 Chemotherapy is not used in kidney cancer. Targeted therapy is based on medications (usually pills) that stop blood supply to the cancer, which slows or stops the growth of the tumour, and sometimes causes it to shrink. These medications target specific signals within the cancer, and are also called “targeted therapies” (see graphic #1).
Chemotherapy is not used in kidney cancer. Targeted therapy is based on medications (usually pills) that stop blood supply to the cancer, which slows or stops the growth of the tumour, and sometimes causes it to shrink. These medications target specific signals within the cancer, and are also called “targeted therapies” (see graphic #1).
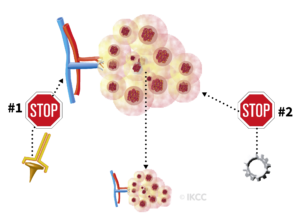
Other names for this group of drugs are “anti-angiogenic therapies” and “tyrosine kinase inhibitors”. While these medications are not chemotherapy, they do have side effects. The tyrosine kinase inhibitors used to treat kidney cancer are: axitinib, cabozantinib, lenvatinib, pazopanib, sorafenib, sunitinib. Another medication, bevacizumab, is an intravenous targeted therapy.
Medications that block cancer’s growth
A second group of medicines for kidney cancer work by blocking a different signal (“mTOR inhibitors”). The mTOR inhibitors (see graphic #2) used to treat kidney cancer are everolimus and temsirolimus.
Immunotherapy with cytokines
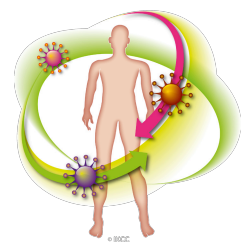 Before 2006, immunotherapy with cytokines such as interleukin-2 (IL-2) and alpha-interferon was commonly used to treat kidney cancer that had spread to other parts of the body (metastatic kidney cancer). These drugs worked for some people by activating killer T cells, which are the part of the body’s immune system that destroys cancer cells. New kinds of immune therapies are becoming available and are being tested in clinical trials.
Before 2006, immunotherapy with cytokines such as interleukin-2 (IL-2) and alpha-interferon was commonly used to treat kidney cancer that had spread to other parts of the body (metastatic kidney cancer). These drugs worked for some people by activating killer T cells, which are the part of the body’s immune system that destroys cancer cells. New kinds of immune therapies are becoming available and are being tested in clinical trials.
Immunotherapy with checkpoint antibodies
Checkpoint antibodies, also called immuno-oncology (IO) therapy (e.g. CTLA-4, PD-1, PD-L1) are the most recent development in the immune therapy of kidney cancer. Immune cells are controlled by a committee of checkpoints which very finely balance the immune system. Too little regulation and the immune system goes overactive and attacks the body; too much and immune functions are impaired and infections and cancers can establish themselves.
Sometimes cancer cells co-opt this system and use checkpoints inappropriately to stop your immune system recognising cancer cells. Checkpoint inhibitors are drugs (in this case antibodies) that in turn block these checkpoints so that the immune system is freed up to fight cancer cells.
Think treatment, think trial
 Many clinical trials are underway around the world that are either specifically for kidney cancer, or that include kidney cancer in the selection criteria.
Many clinical trials are underway around the world that are either specifically for kidney cancer, or that include kidney cancer in the selection criteria.
